What Is EEG and Why Does It Matter in ADHD?
Listen to the Article
For those on the go or who prefer listening, you can play the full audio version of this deep dive below.

For many adults exploring a potential ADHD diagnosis, the journey is filled with uncertainty. You may have spent a lifetime feeling misunderstood and grappling with challenges that others do not seem to face, only to be met with subjective questionnaires. While checklists are an essential part of any assessment, they can feel incomplete on their own. This is where an electroencephalogram, or EEG, enters the conversation. Although it is not a standalone diagnostic tool in the UK, advanced EEG offers invaluable, objective data to support a comprehensive ADHD assessment. It provides a biological window into your brain’s unique activity, moving beyond observation to measurement and validating experiences that have long been dismissed for many people.
Table of Contents
- What Exactly is an EEG?
- The ADHD Brain on an EEG, What’s Different?
- Can You Get an EEG for ADHD on the NHS?
- What Research Says About EEG Accuracy
- Beyond Standard EEG: The Power of qEEG Brain Mapping
- What to Expect During Your EEG Test for ADHD
- Why Trust Eton Psychiatrists?
- Summary
- Sources
- Frequently Asked Questions
What Exactly is an EEG?
An electroencephalogram (EEG) is a medical test used to record the electrical activity of the brain. You can think of it like an ECG for the heart, but for your brain. It functions as a powerful lens, allowing clinicians to observe the intricate symphony of electrical impulses, or brainwaves, that your brain cells use to communicate with one another.
This technology is not new or experimental. For decades, the electroencephalography test has been a cornerstone of neurology, trusted by doctors to diagnose, monitor, and manage conditions like epilepsy, sleep disorders, and other brain-related issues.
The procedure itself is straightforward, completely painless, and non-invasive. It involves placing a series of small metal discs, called electrodes, onto your scalp. These sensors do not send any electricity into your brain. They simply listen, capturing the faint electrical signals your brain naturally produces and transmitting them to a computer. The computer then translates them into the flowing, rhythmic lines of your brain’s electrical conversation.
The ADHD Brain on an EEG, What’s Different?
So, how does this relate to ADHD? Research into the neurobiology of Attention-Deficit/Hyperactivity Disorder suggests that the condition is linked to differences in brain structure, chemistry, and electrical activity. An EEG ADHD analysis can illuminate these differences in a way that conversation alone cannot.
Your brain produces a mixture of brainwaves at different speeds, which are categorised into bands such as Delta, Theta, Alpha, and Beta. Each band is associated with different states of alertness and mental activity. In the context of ADHD, clinicians and researchers are particularly interested in two types.

- Theta Waves are slower brainwaves, dominant during states of deep relaxation, drowsiness, or daydreaming.
- Beta Waves are faster brainwaves, associated with active thinking, focus, problem-solving, and sustained attention.
Neuroscientific studies have identified common patterns in the brains of individuals with ADHD. While every brain is unique, a recurring theme is a difference in the balance of these key brainwaves.
Elevated Theta Wave Activity
Many people with ADHD show an excess of slow-wave Theta activity, particularly in the frontal lobes of the brain. This is the region responsible for executive functions like planning, focus, and impulse control. This can be interpreted as a sign of cortical under-arousal, as if parts of the brain are in a more “daydreamy” state when they need to be focused.
Reduced Beta Wave Activity
Conversely, there is often a deficit of fast-wave Beta activity. This reflects a reduced capacity to maintain a state of focused, attentive concentration, which aligns with the core symptoms of inattention.
Increased Theta/Beta Ratio (TBR)
The relationship between these two brainwave types can be calculated as the Theta/Beta Ratio (TBR). A higher than average TBR is considered a key neurobiological marker, or biomarker, that is strongly correlated with ADHD. In essence, this ratio provides a single, powerful number that captures this signature brainwave pattern of ADHD.
Can You Get an EEG for ADHD on the NHS?
For anyone navigating the diagnostic process in the United Kingdom, this is a critical question. The straightforward answer is that an EEG test is not currently part of the standard diagnostic pathway for ADHD within the NHS. The National Institute for Health and Care Excellence (NICE) guidelines, which set the standard for NHS care, recommend a comprehensive clinical assessment. This typically involves detailed interviews, psychometric questionnaires, and gathering information from family members or school reports where applicable. This process is thorough but remains largely subjective.
You may read about older systems that used EEG data to help diagnose ADHD. While these were important moments for the field, they have not been widely adopted into standard clinical practice here in the UK. Therefore, for individuals seeking this layer of objective data for their assessment, the route is typically through the private sector, where specialist clinics can offer more advanced neurodiagnostic tools.
What Research Says About EEG Accuracy
The question of EEG effectiveness is central to its use in diagnostics. While early use of standard EEG for ADHD was met with scepticism, modern technology has transformed the field. Recent advancements, particularly in computational analysis and machine learning, are overcoming old limitations. A 2025 systematic review published in Clínica y Salud evaluated multiple modern studies and found that EEG-based models consistently achieved high accuracy, with some results reaching up to 99.49%. This powerfully demonstrates the value of EEG not as a replacement for clinical judgement, but as a vital complementary tool that adds a layer of objective biological data.
Further cementing this progress, a 2025 study published in the International Journal of Mental Health and Addiction developed a novel AI model to analyse EEG signals. The model was able to diagnose ADHD with an accuracy of 99.5%, showcasing a remarkable leap in precision. The evidence is clear that the effectiveness of EEG for ADHD is rapidly evolving from a promising theory into a clinical reality.
Beyond Standard EEG: The Power of qEEG Brain Mapping
At leading clinics, the conversation has moved beyond the standard EEG to a far more advanced and detailed technique known as Quantitative Electroencephalogram, or qEEG.
If a standard EEG is like listening to a single instrument in an orchestra, a qEEG is like having the entire musical score. It does not just show the raw brainwaves. It uses sophisticated software to analyse the data, comparing it to a large database of “neurotypical” brains of the same age. This process creates a detailed, colour-coded “brain map” that visually highlights the specific areas of your brain that show unusual patterns of activity.
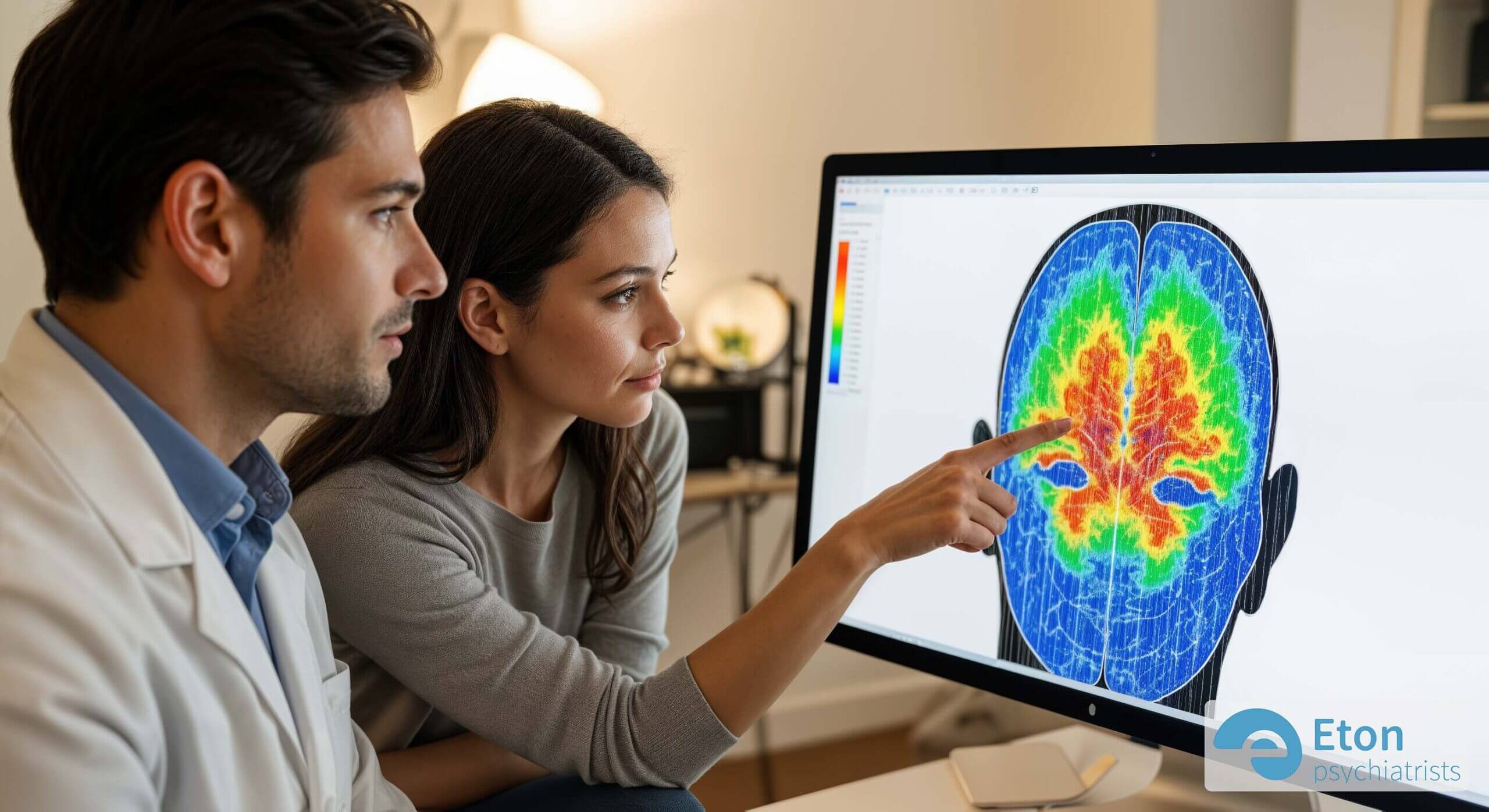
This qEEG brain map is incredibly insightful. It can pinpoint the precise location of under or over-arousal, identify abnormalities in how different parts of the brain are communicating, and provide a level of detail that is simply impossible to achieve with a standard EEG.
Crucially, this level of detail is vital for differential diagnosis. Conditions like Autism Spectrum Disorder (ASD), anxiety, or even the effects of trauma can sometimes present with symptoms that overlap with ADHD. A qEEG brain map can often reveal distinct neurophysiological signatures, helping clinicians to differentiate between conditions and ensure your diagnosis is as accurate as possible.
What to Expect During Your EEG Test for ADHD
The prospect of any medical test can be daunting, but an EEG is a very calm and straightforward procedure. Understanding the process can help alleviate any concerns.
Preparation is minimal. You will typically be asked to ensure your hair is clean, dry, and free from any products like gels, sprays, or oils, as these can interfere with the electrodes’ ability to get a good reading. It is also wise to avoid caffeine on the day of the test.

A trained technician will measure your head and mark the points where the electrodes will be placed. A special gel is used to attach around 20 small sensors to your scalp. This is not in any way painful, though it may feel a little cold or strange. Once the electrodes are in place, you will simply sit back and relax in a comfortable chair. The recording itself may last anywhere from 30 to 60 minutes. You might be asked to open or close your eyes, or look at a flashing light, to see how your brain responds to different stimuli.
Once the recording is complete, the technician will remove the electrodes. Your hair will likely be a little sticky from the paste, but it washes out easily. You can return to your normal daily activities immediately afterwards, as there are no side effects. The recorded data is then processed and analysed by a clinical expert, who will prepare a detailed report for your psychiatrist.
Why Trust Eton Psychiatrists?
At Eton Psychiatrists, we are a CQC-regulated clinic committed to providing the highest standard of mental healthcare. As you can learn on our About Us page, our team is composed of experienced consultant psychiatrists who believe in a holistic and evidence-based approach to diagnosis and treatment. We understand that each individual’s journey is unique, and we integrate advanced diagnostic tools like qEEG with comprehensive clinical assessments to ensure you receive the most accurate and insightful diagnosis possible. Our commitment is not just to clinical excellence, but to providing a supportive and empathetic environment where you feel heard, understood, and empowered.
Summary
- An Objective Tool: The core principle is that while not a standalone diagnostic tool, an EEG (especially an advanced qEEG) provides objective, biological data that validates a person’s experience and complements subjective clinical assessments.
- The ADHD Brain Signature: Research consistently shows patterns in the brains of individuals with ADHD, such as an excess of slow ‘theta’ waves and a deficit of fast ‘beta’ waves, particularly in the frontal lobes. The Theta/Beta Ratio (TBR) is a key biomarker for ADHD.
- UK Diagnostic Pathway: An EEG is not part of the standard NHS pathway for ADHD diagnosis in the UK. Access to this technology is typically through private specialist clinics.
- Advanced qEEG: Quantitative EEG (qEEG) is a more advanced technique that creates a detailed “brain map,” comparing an individual’s brain activity to a normative database. This is powerful for increasing diagnostic accuracy and differentiating ADHD from other conditions.
- The Evidence: Modern research, especially studies using AI analysis, demonstrates high levels of accuracy for EEG in identifying the neural signatures of ADHD, confirming its effectiveness as a complementary diagnostic tool.
Sources
Frequently Asked Questions
Can an EEG definitively diagnose ADHD?
No, not on its own. An EEG for ADHD diagnosis should always be part of a comprehensive assessment conducted by a qualified psychiatrist. The qEEG provides powerful objective data, but that data must be interpreted in the context of your personal history, symptoms, and a full clinical interview.
What does an ADHD brain look like on an EEG scan?
On a qEEG brain map, an ADHD brain often shows an excess of slow-wave (Theta) activity in the frontal regions and a deficit of fast-wave (Beta) activity. This pattern is visually represented as a deviation from the norm, providing a clear picture of the underlying neurobiology of inattentive or hyperactive symptoms.
Is a qEEG test for ADHD accurate?
Modern qEEG analysis, especially when enhanced with AI, has shown very high levels of accuracy in identifying the brainwave patterns associated with ADHD. When used by an experienced clinician as part of a full assessment, it significantly increases the confidence and precision of the final diagnosis.
How much does a private EEG assessment for ADHD cost in the UK?
The cost of a private qEEG assessment can vary depending on the clinic and the comprehensiveness of the report. It is an investment in your health, providing a level of diagnostic clarity that is not available through standard pathways. You should always ensure the provider is reputable and regulated.
How can EEG help with ADHD treatment?
The data from an EEG or qEEG is not just for diagnosis; it can also guide treatment. One of the most exciting applications is in neurofeedback therapy. During neurofeedback, you watch your own brainwave activity in real-time and learn to consciously regulate it, strengthening the neural pathways associated with focus and attention.